CANINE INTERNAL MEDICINE
Canine Internal Medicine
CANINE PANCREATITIS
Pancreatitis is inflammation and swelling of the pancreas. It can occur in a mild or severe form. The cause of spontaneous pancreatitis in dogs is not well understood. Dogs taking corticosteroids may be at increased risk. There is a higher incidence of pancreatitis in dogs with Cushing’s syndrome, diabetes mellitus, hypothyroidism, and idiopathic hyperlipemia (a disease of Miniature Schnauzers). These diseases are all associated with high serum lipid (fat) levels. Pancreatitis is also more prevalent in overweight spayed females and dogs on high-fat diets. An attack may be triggered by eating table scraps, a fatty meal, or dietary indiscretion. We often see this occur especially during holiday parties.
Acute pancreatitis is characterized by the abrupt onset of vomiting and severe pain in the abdomen. The dog may have a tucked-up belly and assume a prayer position. Abdominal pain is caused by the release of digestive enzymes into the pancreas and surrounding tissue resulting in a severe inflammatory reaction diarrhea, dehydration, weakness, and shock often ensue.
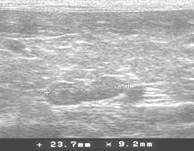
The diagnosis can be suspected based on a physical examination. It is confirmed by blood tests showing elevated amylase and/or lipase levels, along with a new serum test called canine pancreatitic lipase (SPEC cPL). Abdominal ultrasonography is important and often reveals an enlarged and swollen pancreas.
Mild pancreatitis produces loss of appetite, depression, intermittent vomiting, and diarrhea and weight loss, whereas fulminant necrotizing pancreatitis is an acute, extremely severe, usually fatal form of pancreatitis. These dogs become more and more severely ill and painful to the point of collapse. Dogs may vomit or simply show signs of severe abdominal pain. If you suspect your dog has pancreatitis, please get your dog to our office immediately.
Following an attack of pancreatitis, the pancreas may be permanently damaged. If the pancreatic islet cells (produce insulin) have been damaged diabetes mellitus may occur; or if the pancreatic acinar cells (produce digestive enzymes) have been affected exocrine pancreatic insufficiency or digestive problems may occur.
Treatment: Dogs with acute pancreatitis require hospitalization to treat shock and dehydration. The most important step in treating pancreatitis is to rest the gland completely and adequate hydration. This is accomplished by giving the dog nothing by mouth for several days and maintaining fluid and electrolyte balance with intravenous fluid solutions. Antibiotics are used to prevent secondary bacterial infections. Pain is controlled with narcotics. Cardiac arrhythmias, if present, are treated with anti-arrhythmic drugs.
Dogs who do not respond to medical treatment may require surgery to drain an infected pancreas. The prognosis for dogs with shock and spreading peritonitis is poor.
Dogs who recover from pancreatitis are susceptible to recurrent attacks, which can be mild or severe. These episodes can be prevented, in part, by eliminating predisposing factors. For example, place overweight dogs on a weight-loss program. Feed the total daily ration in two or three small servings to avoid over stimulating the pancreas. Do not feed table scraps. Dogs with high serum lipid levels (determined by lab tests) should be placed on a fat-restricted diet. If scarring has damaged the acinar or islet cells, your dog may need supplemental treatment such as digestive enzymes or insulin.


CANINE HYPOTHYROIDISM
Hypothyroidism is a clinical state associated with inadequate production of thyroxine (thyroid hormone), which causes lowered cellular metabolism in most tissues of the body. The most common form in the dog is primary hypothyroidism 95%, which results from significantly decreased hormone production by the thyroid gland due to an inflammatory disease or simple loss of function. Clinical signs usually develop during middle age (4 to 10 years). They tend to occur at an earlier age in breeds at increased risk including Golden Retrievers, Doberman Pinschers, Dachshunds, Irish Setters, Schnauzers, Great Danes, Poodles, and Boxers.
The signs vary and depend in part on the age of the animal. In adult dogs, the most consistent clinical signs of hypothyroidism result from decreased cellular metabolism and its effects on the animal’s mental status. Most show some mental dullness, lethargy, exercise intolerance or unwillingness to exercise, a propensity to gain weight without an increase in appetite or food intake, and cold intolerance. These signs are often gradual in onset, subtle, and not frequently recognized by the owner until questioned by a veterinarian. Additional indications typically involve the skin and, less commonly, the neuromuscular system.
Dermatologic alterations include hair loss on both sides of the body that tend to spare the head and extremities. It may be localized or generalized and can involve only the tail (“rat tail”). Seborrhea (dry or oily skin) and pyoderma (skin infection) are also common signs. Lastly, the hair coat is often dull, dry, and easily pulled out. Hair regrowth is often very slow. Chronic ear infections have also been noted. Less common manifestations include eye, cardiovascular, and gastrointestinal abnormalities.
Hypothyroidism is relatively easily treated and routinely diagnosed with blood chemistries. Occasionally, additional testing may be required to accurately diagnose the condition. The treatment of choice is daily synthetic thyroid hormone supplementation in the form of tablets. Once an animal is started on supplementation, improvement in activity and attitude is usually noted within 7-10 days. Visible improvement in skin and hair coat may take 6-8 weeks or longer. Follow-ups include rechecking thyroid levels 4-6 hours post-pill in 3-4 weeks. Frequently, the dosage may need to be changed and rechecked during the first 3 months of treatment. Once the proper dose is identified, lifelong administration is required with periodic thyroid level checks 1-2 times yearly.


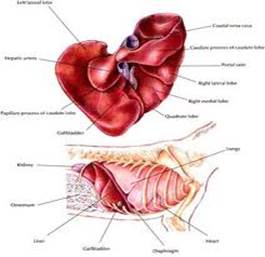
CANINE LIVER DISEASE
The early signs of liver disease are nonspecific. They include loss of appetite, weight loss, and chronic intermittent vomiting and diarrhea. Vomiting is more common than diarrhea. Drinking and urinating more often than normal may be the first signs, and the principal reason for seeking medical attention.
In the early stages of liver disease the liver swells and enlarges. As the disease progresses, the liver cells die and are replaced by scar tissue. The liver then becomes rubbery and firm. This condition is called cirrhosis. It is not reversible. Before the liver reaches this terminal stage, it can recover from damage and heal itself to the point where your dog has normal liver function. This is possible if proper treatment is instituted early on; the extent of recovery depends on the exact cause of the liver damage. Eighty percent of liver cells must die before the liver begins to fail. The signs of liver failure are jaundice, hepatic encephalopathy, ascites (abdominal fluid), spontaneous bleeding, and dependent edema-swollen lower limbs. Treatment of liver failure is directed toward treating the liver disease that is causing it.
Jaundice
With impaired liver function, bile accumulates in the blood and tissues, staining the tissues yellow. This can be seen in the yellow appearance of the white of the eyes and in the mucous membranes of the gums and tongue. The inside of the ears is another area where yellow pigment can be detected. Bile excreted in the urine turns the urine dark brown (the color of tea). Jaundice may also result from the breakdown of large numbers of red blood cells, such as in acute hemolytic anemia. Post hepatic bile duct obstruction can also cause jaundice.
Hepatic Encephalopathy
This is a type of brain dysfunction caused by high levels of ammonia and other toxins in the blood. Ammonia is a byproduct of protein metabolism, and is normally removed from the bloodstream by a healthy liver. When the liver is sick, ammonia accumulates to toxic levels and exerts a poisonous effect on the brain.
Dogs with hepatic encephalopathy develop incoordination, sporadic weakness, disorientation, head-pressing, behavioral changes, drooling, stupor, and mental dullness. Symptoms tend to wax and wane. They become more severe after a high-protein meal. Seizures and coma occur when hepatic encephalopathy is advanced.
Ascites
Ascites is the accumulation of fluid in the abdomen. In a dog with liver disease, it is caused by low serum proteins and increased pressure in the veins that supply the liver. A dog with ascites has a swollen or bloated look. Thumping on the abdomen produces a dull, flat sound.
Bleeding
Spontaneous bleeding occurs in dogs with advanced liver disease. Common sites of bleeding are the stomach, intestines, and urinary tract. Blood may be noted in the vomitus, stools, or urine. Punctate (pinhead-size) hemorrhages may be seen on the gums. Bruises can appear under the lips and skin. Major blood loss from spontaneous bleeding is relatively uncommon, but uncontrollable bleeding can be a serious problem if the dog is injured or requires surgery.
Causes of Liver Disease
A number of diseases, chemicals, drugs, and toxins can damage the liver. The liver is directly affected by infectious canine hepatitis and leptospirosis. It is frequently involved in heartworm infection, Cushing’s syndrome, and diabetes mellitus. Primary and metastatic tumors are a major cause of liver failure in dogs. Chemicals known to produce liver toxicity include carbon tetrachloride, insecticides, and toxic amounts of lead, phosphorus, selenium, arsenic, and iron. Drugs capable of damaging the liver include anesthetic gases, antibiotics, antifungals, dewormers, diuretics, analgesics (including NSAIDs), anticonvulsants, testosterone preparations, and corticosteroids. Most drug reactions are associated with excessive dosage and/or prolonged use.
Some plants and herbs can also cause liver failure; these include ragwort, certain mushrooms, and blue-green algae. Molds such as aflatoxin, which grows on corn and may contaminate foods, can cause severe liver damage.
A blockage of the bile duct by gallstones, liver flukes, tumors, or pancreatitis is uncommon, but becomes a consideration when a dog has unexplained jaundice.
Treatment: Blood tests, including bile acid assay, ultrasound, and CT scan, provide useful information, but the only definitive test is biopsy of the liver. The prognosis for recovery depends on how long the dog has been ill, the extent of liver damage, and whether the disease can be surgically cured or controlled with medications.
Infectious diseases respond to treatment of the underlying condition. Drugs and poisons frequently exert temporary effects that are reversed when the exposure is stopped. Bile duct obstructions and some primary tumors of the liver can be corrected by surgery.
In addition to treating the liver disease, it is important to control and prevent complications, particularly hepatic encephalopathy and bleeding. This may involve feeding a special diet that is low in protein, lowering blood ammonia levels, maintaining blood-clotting factors, preventing seizures, correcting electrolyte abnormalities, and administering antacids to prevent stomach and duodenal ulcers. Supplements such as SAM-e and milk thistle are useful in both restoring and maintaining normal liver.


CANINE KIDNEY DISEASE
Kidney failure is defined as the inability of the kidneys to remove waste products from the blood. The buildup of toxins produces the signs and symptoms of uremic poisoning. Kidney failure can appear suddenly (acute kidney failure) or come on gradually over months. Most cases are of the gradual onset type and are caused by nephritis and nephrosis.
Causes of acute kidney failure include:
- Complete urinary tract obstruction caused by a stone
- Rupture of the bladder or urethra
- Shock, with inadequate blood flow to the kidneys
- Congestive heart failure with low blood pressure and reduced blood flow to the kidneys
- Poisoning, especially from antifreeze, grapes and raisins, and recently some chicken strip treats from China
- Leptospirosis (an infectious disease)
Dogs with kidney failure do not show signs of uremia until 75 percent of functioning kidney tissue is destroyed. Thus, a considerable amount of damage occurs before the signs are noticed.
Signs of Kidney Failure
One of the first things you may notice is that your dog drinks and urinates more than usual and indicates her need to go outside to eliminate several times a day. If not allowed to do so, the dog may begin to have housetraining accidents in the house. These signs are due to the failure of the kidneys to concentrate the urine. This results in a large urine output over which the dog has no control, with subsequent dehydration and thirst.
As kidney function declines, the dog retains ammonia, nitrogen, acids, and other chemical wastes in the blood and tissues. This is called uremia. The degree of uremia is determined by measuring serum blood urea nitrogen (BUN), creatinine, and electrolytes.
Signs of uremia are apathy and depression, loss of appetite and weight, a dry hair coat, a brownish discoloration to the surface of the tongue, and an ammonia-like odor to the breath. Dogs at this stage may urinate less than normal. Ulcers may arise in the mouth. With the nephrotic syndrome the dog develops ascites (abdominal fluid) and edema. Vomiting, diarrhea, and gastrointestinal bleeding may occur. At the end stages of kidney failure, the dog falls into a coma.
Treating Kidney Failure
Dogs with kidney failure require periodic monitoring of blood chemistries to detect changes in kidney function that may require medical intervention. A most important step is to restrict salt intake. This helps prevent edema, ascites, and hypertension.
Protein is poorly metabolized by dogs with kidney failure, but what to do about protein levels in the diet is currently an area of controversy. Some veterinarians believe a diet rich in meat, or one that contains poor-quality protein, creates an increased nitrogen load that must be handled by the liver and kidneys. Dogs with weak kidneys can be thrown into uremia by feeding them more protein than they can handle. Other veterinarians believe that as long as the protein is of high biological value, it will help the kidneys retain their function. Diet may need to be customized to the individual dog.
Restricting phosphrus intake is agreed upon by all. Medications to lower phosphorus levels may be required along with dietary adjustments.
It is extremely important to provide fresh water at all times. The dog must be able to take in enough water to compensate for her large urine output. Some dogs will need occasional boosts to their fluid intake. This can be done by giving subcutaneous (known as sub-Q or SQ) fluids. With most dogs, their owners can learn how to do this at home. In the later stages of kidney failure, dogs may need sub-Q fluids daily.
Some types of kidney failure are acute, and are mild enough that if the dog is well supported medically, there will be a good recovery. More commonly, dogs will have at least some renal function deficit and need a change in care for the rest of their lives. With chronic renal failure, there is no cure; the disease must be controlled as well as possible for the rest of the dog’s life.
Dialysis
Dialysis describes two therapies that try to duplicate the filtering tasks of the kidneys. In peritoneal dialysis, special fluid is put into the abdomen using a catheter. The fluid then washes tissues and absorbs toxins from the body across tissue barriers. After a set period of time, the fluid is removed through the same catheter, taking the toxins out with it. This technique has been used in veterinary referral centers for short-term kidney problems such as antifreeze poisonings.
Hemodialysis is the second technique. This therapy is only available at a few referral centers across the country, because the equipment is expensive and must be specially designed to work with dogs. The dog’s blood is circulated through a machine with filters duplicates the filtering tasks of a healthy kidney.
Kidney Transplant
Another option for dogs with terminal kidney failure is to consider a kidney transplant. Kidney transplants are only done a few veterinary referral centers, but are becoming more common. As with human transplant patients, drugs must be given post-transplant to prevent organ rejection. These drugs are quite expensive and must be carefully calibrated to minimize side effects.






CANINE CUSHING’S DISEASE
The adrenal glands are small, paired structures located just above each kidney. The outer zone of the adrenal gland (the cortex) is composed of glandular cells that manufacture and release corticosteroids. There are two types of corticosteroids: mineralocorticoids and glucocorticoids. Mineralocorticoids regulate electrolyte concentrations. Glucocorticoids reduce inflammation and suppress the immune system. Glucocorticoids are the type of corticosteroids used in nearly all steroid medications. The output of corticosteroids from the adrenal glands is controlled by the pituitary gland through the production of adrenocorticotropic hormone (ACTH).
Cushing’s syndrome is a disease caused by long-term exposure to high levels of glucocorticosteroids, either manufactured by the body or given as medications.
Tumors of the pituitary gland that secrete ACTH stimulate the adrenal glands to produce large amounts of adrenal hormones. This sustained overproduction in response to pituitary stimulation accounts for 85 percent of cases of spontaneous Cushing’s syndrome. The remaining 15 percent are caused by corticosteroid-producing tumors of the adrenal glands themselves. Spontaneous Cushing’s syndrome occurs primarily in middle-aged and older dogs, although dogs of all ages can be affected. Poodles, Boston Terriers, Dachshunds, and Boxers have the highest incidence. A number of cases of Cushing’s syndrome are caused by long-term therapy with drugs that contain corticosteroids. This is called iatrogenic Cushing’s syndrome.
Excess cortisone can cause hair loss over the body in a symmetric pattern, with darkening and in late stages calcification of the underlying skin. The remaining hair is dry and dull. Small blackheads may be found on the abdomen. The abdomen is pendulous, distended, and pot-bellied. Other signs include lethargy with reduced activity, infertility in females, testicular atrophy and infertility in males, loss of muscle mass, and weakness. Excessive thirst and frequent urination also occur.
Dogs with hyperadrenocorticism lose body condition and develop severe problems such as hypertension, congestive heart failure, and diabetes mellitus. Other complications include increased susceptibility to infections, blood clots in the circulatory system (thromboembolism), and central nervous system signs including behavioral changes and seizures.
The diagnosis of Cushing’s syndrome is based on laboratory tests, especially those that measure serum cortisol concentrations before and after the injection of ACTH and dexamethasone. Advances in CT scans and magnetic resonance imaging (MRI) techniques have made it possible to visualize small tumors of the pituitary and adrenal glands. Ultrasound can also be used to measure the size and symmetry of the adrenal glands.
Treatment: Spontaneous Cushing’s syndrome is treated with mitotane or trilostane. Mitotane acts on the adrenal cortex to selectively suppress the production of glucocorticoids. The drug protocol is complex, costly, and requires close veterinary monitoring. Treatment with the newer medication trilostane (Vetoryl) that blocks the production of cortisol is easier and often has fewer complications and as a result is often less costly to use. The prognosis for Cushing’s disease is guarded. The average life span with medical treatment is about two years, although longer survival is common with the use of trilostane. Benign and malignant tumors of the adrenal glands can be surgically removed in some cases. Iatrogenic Cushing’s syndrome is often reversible if the causative drug can be tapered and, preferably, discontinued. If your dog is on long-term corticosteroids for a medical condition and develops signs of hyperadrenocorticism, your veterinarian may be able to reduce the dosage or find a substitute medication.
Classic Cushing’s Disease Findings


CANINE DENTISTRY
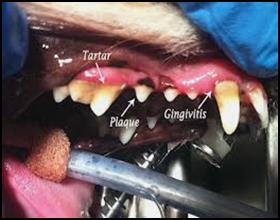
Everyone can understand the importance of dental care for their pets, because the risk of gingivitis and periodontal disease is the same for animals as it is for people. Dental disease is the most common medical problem seen in routine canine practice. There is no reason to believe that animals do not feel the same pain of sore gums and a toothache that we feel. So, the main reason to care for your pet’s teeth is to prevent pain.
If you never brushed your teeth, your mouth would be sore and you would have trouble eating. You might feel tired all the time because the infection in your mouth would spread throughout your body. The exact same thing happens in your pet’s mouth. The mouth is the door to the rest of the body. It has a very good immune system to protect it against the constant barrage of bacteria and toxins it deals with every minute. But it needs some help. We must keep it clean of the plaque that is constantly forming on the teeth.
Plaque is a clear, thick substance consisting of saliva, bacteria, and food particles. In fact, plaque is 80% bacteria and forms within 6-8 hours after brushing. It sticks to the teeth and collects in the pockets around the teeth. If not removed, an infection will result. This infection will eventually overwhelm the body’s immune system. This dental plaque also leads to bad breath, gum disease, and eventually leads to tartar/calculus accumulation, and eventual periodontal disease and loss of teeth. More importantly, tartar and plaque are also linked to more serious problems, such as liver, kidney, joint disease, and heart disease. Routine dental care may save more than your pet’s smile, therefore, dental exams and cleaning are recommended annually.
Pet dentistry has become an established aspect of good veterinary care.
And for good reason!
Ten Steps to Your Dog’s Dental Health
Did you know that regularly brushing your dog’s teeth and providing her with a healthy diet and plenty of chew toys can go a long way toward keeping her mouth healthy? Many pooches show signs of gum disease by the time they’re four years old because they aren’t provided with proper mouth care—and bad breath is often the first sign of a problem. Give your dog regular home checks and follow the tips below, and you’ll have a very contented pooch with a dazzling smile.
- The Breath Test
Sniff your dog’s breath. Not a field of lilies? That’s okay—normal doggie-breath isn’t particularly fresh-smelling. However, if his breath is especially offensive and is accompanied by a loss of appetite, vomiting or excessive drinking or urinating, it’s a good idea to take your pooch to the vet.
- Lip Service
Once a week, with your dog facing you, lift his lips and examine his gums and teeth. The gums should be pink, not white or red, and should show no signs of swelling. His teeth should be clean, without any brownish tartar.
- Signs of Oral Disease
The following are signs that your dog may have a problem in his mouth or gastrointestinal system and should be checked by a veterinarian:
- Bad breath
- Excessive drooling
- Inflamed gums
- Tumors in the gums
- Cysts under the tongue
- Loose teeth
- The Lowdown on Tooth Decay
Bacteria and plaque-forming foods can cause build-up on a dog’s teeth. This can harden into tartar, possibly causing gingivitis, receding gums and tooth loss. One solution? Regular teeth cleanings, of course.
- Canine Tooth-Brushing Kit
Get yourself a toothbrush made especially for canines or a clean piece of soft gauze to wrap around your finger. Ask your vet for a toothpaste made especially for canines or make a paste out of baking soda and water. Never use fluoride with dogs under six months of age—it can interfere with their enamel formation. And please do not use human toothpaste, which can irritate a dog’s stomach. Special mouthwash for dogs is also available—ask Dr. Innes.
- Brightening the Pearly Whites
Taking these steps will make brushing a lot easier for the both of you:
- First get your dog used to the idea of having her teeth brushed. Massage her lips with your finger in a circular motion for 30 to 60 seconds once or twice a day for a few weeks. Then move on to her teeth and gums.
- When your pooch seems comfortable being touched this way, put a little bit of dog-formulated toothpaste or a paste of baking soda and water on her lips to get her used to the taste.
- Next, introduce a toothbrush designed especially for dogs—it should be smaller than a human toothbrush and have softer bristles. Toothbrushes that you can wear over your finger (or a clean piece of gauze) are also available and allow you to give a nice massage to your dog’s gums.
- Finally, apply the toothpaste to her teeth for a gentle brushing, as in step 7.
- A veterinary exam beforehand may be helpful to find out if your dog’s gums are inflamed. If your dog has mild gingivitis, brushing too hard can hurt her gums.
- Brushing Technique
Yes, there is actually a technique! Place the brush or your gauze-wrapped finger at a 45-degree angle to the teeth and clean in small, circular motions. Work on one area of your dog’s mouth at a time, lifting her lip as necessary. The side of the tooth that touches the cheek usually has the most tartar, and giving a final downward stroke can help to remove it. If your dog resists having the inner surfaces of her teeth cleaned, don’t fight it—only a small amount of tartar accumulates there. Once you get the technique down, go for a brushing two or three times a week.
- Know Your Mouth Disorders
Getting familiar with the possible mouth problems your dog may encounter will help you determine when it’s time to see a vet about treatment:
- Periodontal disease is a painful infection between the tooth and the gum that can result in tooth loss and spread infection to the rest of the body. Signs are loose teeth, bad breath, tooth pain, sneezing and nasal discharge.
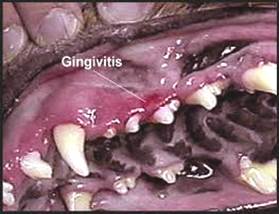
- Gingivitis is an inflammation of the gums caused mainly by accumulation of plaque, tartar and disease-producing bacteria above and below the gum line. Signs include bleeding, red, swollen gums and bad breath. It is reversible with regular teeth cleanings.
- Halitosis—or bad breath—can be the first sign of a mouth problem and is caused by bacteria growing from food particles caught between the teeth or by gum infection. Regular tooth-brushings are a great solution.
- Swollen gums develop when tartar builds up and food gets stuck between the teeth. Regularly brushing your dog’s teeth at home and getting annual cleanings at the vet can prevent tartar and gingivitis.
- Proliferating gum disease occurs when the gum grows over the teeth and must be treated to avoid gum infection. An inherited condition common to boxers and bull terriers, it can be treated with antibiotics.
- Mouth tumors appear as lumps in the gums. Some are malignant and must be surgically removed.
- Salivary cysts look like large, fluid-filled blisters under the tongue, but can also develop near the corners of the jaw. They require drainage, and the damaged saliva gland must be removed.
- Canine distemper teeth can occur if a dog had distemper as a puppy. Adult teeth can appear looking eroded and can often decay. As damage is permanent, decayed teeth should be removed by a vet.
- Chew on This
Chew toys can satisfy your dog’s natural desire to chomp, while making his teeth strong. Gnawing on a chew toy can also help massage his gums and help keep his teeth clean by scraping away soft tartar. Ask your vet to recommend toxin-free rawhide, nylon and rubber chew
toys.
P.S.: Gnawing also reduces your dog’s overall stress level, prevents boredom and gives him an appropriate outlet for his natural need to chew.
10. Diet for Healthy Teeth – There are many veterinary prescription diets that can
significantly help decrease plaque build-up and the onset of dental disease.
Ask Dr. Innes or staff for more information.
In the sections below, please find information on some of the more common dental/oral conditions that we see in our general dental practice. There are of course may other severe dental/oral conditions that are not noted here. If you have any concerns about your dogs dental health please contact our office and schedule an appointment with Dr. Innes. There is also some further information about dental home care at the end of the section.
Method and Equipment
Advanced Equipment
We use an advanced human piezo-electric dental scaler (most vets use a simpler ultrasonic scaler) that allows us to clean teeth thoroughly and efficiently. The various tips allow for removal of large amounts of tartar as well as more delicate cleaning below the gum margin. We also use hand scalers when needed and then polish the teeth just like when you have your teeth cleaned. Lastly, a sealant can be applied to the teeth to help prevent further plaque build-up.
Our dental table includes both high- and low-speed drills when needed for extractions
All of our surgical equipment is steam sterilized for each patient.
Anesthesia
Anesthesia is an area of concern for most pet owners. We examine your pet and his or her medical history to develop a protocol specifically for them. This often includes routine blood work to ensure there are no underlying liver, kidney, infections, anemia, or other physiological problems that could put your pet at risk for anesthesia.
We use state-of-the-art monitoring equipment that includes ECG, oxygen saturation of the blood, carbon dioxide levels, blood pressure and temperature.
Dr. Innes has two decades of experience monitoring patients under anesthesia.
There are various pre-anesthetic medications that are utilized, depending on the dog’s size and Dr. Innes’ preference. After the animal is relaxed general anesthesia is induced. This, too, can be in various forms. One under general, an endotracheal tube is placed to provide a “safe” airway so anesthesia can be maintained with 100% oxygen and human grade anesthetic gas.
Inside the mouth, we utilize lidocaine gel along the gum margin and local anesthetic blocks to reduce pain and allow us to keep our general anesthesia level as low as possible. Your pet’s safety and comfort are of paramount importance to us.

Gingivitis and Periodontal Disease
Periodontal disease is a disease of the tissues that support the teeth in the mouth. Both bacterial infection and inflammation play a role in this pervasive disease of dogs, cats and people. These tissues are the gums, the jaw bone, and the periodontal ligament which connects the tooth to the bone. Periodontal disease occurs when the body’s immune system reacts to the bacteria and toxins which are constantly forming on the teeth in the form of plaque.
If plaque is not removed, it will eventually accumulate and harden into dental calculus also called tartar. Calculus can become a hard yellow brownish covering over the crowns of the tooth. It’s like cement and is difficult to remove. With heavy build-up, calculus can also cover the gum so that the plaque beneath the gum-line cannot be cleaned. This build-up exacerbates the situation, creating a nice environment in which the nastiest plaque bacteria thrive. The plaque beneath the gum-line is the real enemy in periodontal disease. Fortunately plaque that is above the gumline is removeable with tooth brushing.
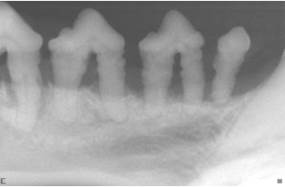

| The pictures above show what severe calculus and periodontal disease look like visually and with digital radiographs. Note there is severe bone loss around the tooth roots. |
As the plaque accumulates and the bacteria multiply, the pockets around each tooth become deeper and more painful for your pet. An early sign of this stage is a swelling and reddening at the gum-line around each tooth. If you touch this area, your pet may shy away and the gums may bleed. This is gingivitis, the earliest form of periodontal disease. Gingivitis is a reversible inflammation of the gums. If the teeth and gums are cleaned now, the mouth can be “as good as new.” However, if the pockets around the teeth are deep enough, the gums recede, or the bone supporting the teeth begin to resorb, irreversible changes have occurred in the mouth. This is advanced periodontal disease. At this stage the disease can be arrested, but the damage it has caused cannot be completely reversed.
Discolored Teeth
A discolored tooth can occur after trauma. Typically this happens when a pet chews on hard objects or from blunt trauma to the mouth. The pulp of the tooth bleeds and initially stains the dentin pink. Eventually the tooth will become a purple or grey.
A study reported in the Journal of Veterinary Dentistry by Dr. Fraser Hale (JVD, Vol18:1, March 2001 and the Veterinary Dental Forum in October 2001) showed that 94% of discolored teeth suffer from partial or total pulp necrosis and only 58% of those show radiographic signs of necrosis. The study concluded that discolored teeth need to be either extracted or treated with root canal therapy.
We recommend that discolored teeth (even partially discolored) are either extracted or treated with root canal therapy. If you suspect that your cat or dog has a discolored tooth, please contact our office to schedule an appointment with Dr. Innes.

Fractured Teeth
Just like humans, pets can break their teeth. A tooth fractures due to trauma, such as chewing on something that is too hard. The most common causes of fractured teeth that we see are: cow hooves, hard nylon toys, ice cubes, rocks, and marrow bones. A fractured tooth with pulp exposure allows bacteria to enter the tooth, leading to pain and infection. Often a stoic animal may not show outward signs of oral pain but will show dramatic signs of improvement once the tooth is treated surgically. It is not unusual for an owner to be unaware that their pet has a fractured tooth until the infection has become so bad that it causes facial swelling. Antibiotics will help to temporarily treat the infection, but once the medication is stopped, the infection will return. We always recommend treating a fractured tooth with pulp exposure either with root canal therapy or extraction. If you suspect that your cat or dog has a broken tooth please contact our office for an appointment with Dr. Innes


Extractions are another area of concern for pet owners. We try and keep as many teeth in your pet’s mouth as possible, but leaving a diseased tooth behind would lead to continue discomfort and systemic effects for your pet.
When extractions are necessary, like the fractured teeth seen above or teeth with severe periodontal disease, we start with long acting (6-8 hours) local anesthetic blocks to “numb” the area where the tooth is to be extracted. In addition, opiod pain medications and antibiotics are administered. We then perform surgical extractions that result in less trauma and faster healing with the surgical opening closed with absorbable sutures.
Broken and Retained Deciduous Teeth
Broken and retained deciduous teeth should also be extracted. The teeth that are present around 6 weeks of age are not the permanent teeth the puppy will have as an adult. Like humans, dogs have two sets of teeth that develop during their lifetime. The first set of teeth, sometimes called “baby” teeth are also called deciduous teeth because these teeth are present early in life, and then are shed as the developing permanent teeth erupt into position. Deciduous teeth are typically lost or shed as the roots of these teeth are resorbed and the crown becomes loose. If the deciduous tooth is not shed in a timely manner, we refer to them as “retained”. Retained deciduous teeth should be removed, provided there is a permanent tooth to replace it.
Deciduous teeth in puppies are usually present at 5-6 weeks of age and are lost between 3-6 months. One of the best times to evaluate for retained deciduous teeth is at the time of the spay or neuter surgery. Since the pet will already be under anesthesia, this creates an excellent opportunity to remove any retained deciduous teeth that might cause further problems. The root of a deciduous tooth is amazingly large. What you see of a deciduous tooth above the gumline is only about 25% of the entire tooth.
As a general rule of thumb, there should only be one tooth occupying a specific place. More simply put, if there is a permanent tooth that has erupted through the gingiva and a deciduous tooth remains, the deciduous tooth should be removed to prevent possible deflection of the permanent tooth’s eruption path, or to prevent crowding of the two involved teeth, which could lead to periodontal problems that could affect the permanent tooth.

A retained canine tooth with severe dental disease that is now affecting the adult tooth
Oronasal Fistula
An oronasal fistula is a hole in the palatal oral soft tissue and bone that communicates with the nasal sinus. They can be caused by trauma, such as a maloccluded tooth or from periodontal disease. Dachshunds are commonly affected by oronasal fistulas secondary to periodontal disease of their upper canine teeth. Pets will frequently sneeze or reverse sneeze because food and other debris becomes lodged in their nose. Also owners might notice a discharge from either one or both nostrils. An oronasal fistula will not heal on its own and does require surgical intervention. If your pet is sneezing or having nasal discharge and you suspect an oronasal fistula, please contact our office to schedule an appointment with Dr. Innes.


Oral Tumors
The words “tumor” or “cancer” strike fear into pet owners and for good reason. Fortunately, the term tumor does not always mean a mass that will spread throughout the body. Tumor can mean a benign mass, that is one that does not spread to other parts of the body, or malignant, which means a mass that has the potential to spread to other areas. All tumors behave differently based on their type with some never spreading, some invading the tissues where they are, and some spreading out within the local tissues and spreading to other areas of the body.
Oral neoplasias (tumors) account for 6% of all tumors in dogs and 10% of all tumors in cats. Of these, 50% are malignant in dogs and 90% are malignant in cats. Many oral masses look alike, whether benign or malignant. The key to successful treatment planning is early detection and microscopic evaluation (biopsy) of all oral masses. Small lesions may seem insignificant due to their size, but if the mass turns out to be malignant, obtaining adequate surgical margins without major structural loss is much easier with lesions less than 1 cm than those larger. In most cases, complete surgical removal of oral tumors early in the course of disease is the preferred treatment. Dental radiographs can be a valuable diagnostic tool when evaluating oral masses.
In general, benign tumors do not typically invade bone, as such, these lesions tend to deflect teeth and alter their position. On the other hand, malignant masses can be invasive into bone, and usually remove bone around tooth roots without displacing teeth. Notation of lymph node size and consistency along with chest x-rays, abdominal ultrasound, and other diagnostic modalities such as Computed Tomography (CT) or Magnetic Resonance Imaging (MRI) can also be helpful especially when staging oral tumors. Most benign lesions can be removed with small surgical margins extending into clinically healthy tissue only. The exception to this rule is the acanthomatous epulis (aka acanthomatous ameloblastoma, central odontogenic fibroma, adamantanoma). These tumors are technically benign because they have never been shown to spread to other organs, but they can invade into the bone surrounding teeth. The acanthomatous epulis is also very sensitive to radiation therapy. Treatment with either radiation therapy or surgical removal with clean margins carries an excellent prognosis (95+%).
Malignant tumors require 1-2cm surgical margins into clinically and radiographically healthy tissue. The most common oral malignancies in dogs are the malignant melanoma, fibrosarcoma, and squamous cell carcinoma. By far and away, the squamous cell carcinoma is the most common oral malignancy in the cat. If caught early, many of these oral tumors can successfully be removed surgically. Those with higher potential to spread should have continued monitoring for early detection of other tumors. Regional lymph node aspirate prior to surgery or lymph node excision is advocated. Consultation with an oncologist with any malignancy is also recommended to consider all treatment options. These pictures show the typical presentation of oral masses. If your dog has an oral growth like this, please call our office ASAP!


Pet Dental Home Care Recommendations
It is very important to your pet’s health to receive regular dental home care just as you take care of your own teeth. Animals have no special ability to resist dental disease. Please read the following guidelines to help assist you in achieving a successful dental home care program for you and your pet.
Step 1: Examine and Touch the Mouth, Teeth, and Gums
The first step is to make it fun and relaxing for your pet. Use lots of praise and start slowly. Begin by offering a small amount of flavored pet toothpaste on your index finger as “a treat” daily for 5-7 days. This conditions your pet to expect a treat when they see the tube of toothpaste.
Step 2: Brushing or wiping the Teeth with Pet Toothpaste
After this initial introductory period, as you give the paste, use your index finger to rub the teeth and gums in small circles, the same motion as a toothbrush. Continue this for 5-7 days. Once your pet becomes comfortable with this, then progress to a soft bristle brush and continue the same routine. You may want to offer a small amount of the paste before and after brushing as a reward. Some pets will require daily brushing, while others can be maintained by brushing a few times a week.
*** Human toothpaste is not meant to be swallowed and should NOT be used on your pet.
Step 3: Mouth Rinses
Pets with advanced periodontal disease or pets that will not allow brushing may also benefit from an antiseptic oral rinse. These rinses are not as well liked as the flavored toothpastes and will not remove plaque as well as brushing, but they will help reduce plaque bacteria.
Step 4: Treats
There are products that have been proven in clinical trials to reduce plaque and tartar accumulation. Look for the Veterinary Oral Health Council (V.O.H.C.) Seal of Approval on products to ensure that are beneficial for your pet’s dental health.
*** Avoid hard treats such as real bones, hard plastic bones, and cow hooves as they can lead to broken teeth.
Step 5: Diets
Specially formulated diets are available that help reduce plaque and tartar build-up. ROYAL CANIN diets have added chemicals that retard the mineralization of plaque to tartar, thus making the teeth easier to keep clean. Other diets such as Hill’s Prescription t/d diet works mechanically to “brush” the teeth when chewing. The t/d diet can be fed as the sole diet, or as treats.
If you find you cannot perform dental home care on your pet, and you want to keep your pet healthy and avoid bad breath and dental disease, you MUST seek professional treatment more frequently! For most pets a professional cleaning once a year is adequate. Pets with pre-existing dental disease and those lacking dental home care will need professional care more often.

CANINE HEART DISEASE
Degenerative Valvular Disease
Chronic degenerative valvular disease is the most common acquired heart disease in dogs. Also known as endocardiosis or myxomatous valvular degeneration, degenerative valvular disease is more common in older small breed dogs. Males appear to be at an increased risk of developing a potentially more severe form of the disease. Previous studies show the following breeds are prone to degenerative valvular disease: poodle (miniature and toy), miniature schnauzer, cocker spaniel, Chihuahua, fox terrier, dachshund, Boston terrier, Doberman pinscher, and Cavalier King Charles spaniel. The underlying cause of degenerative valvular disease is unknown, but previous papers support a heritable etiology in some breeds i.e. Cavalier King Charles spaniels and dachshunds.
The atrioventricular valves (AV valves) separate the top and bottom chambers of the heart. They are composed of leaflets and supporting structures (chordae tendineae) that attach the leaflets to the papillary muscles. The mitral valve is located on the left side of heart and is affected in ~60% of cases with the tricuspid valve (right side of the heart) solely affected ~10% of the time. Approximately 30% of cases involve both AV valves. Rarely the disease affects the aortic and pulmonic valves.
Lesions associated with the disease include: redundant valve leaflets, lengthening of the chordae tendineae, and thickened/fenestrated valve leaflets. This is due to one layer of the valve tissue thickening while another area is degenerating. As a result, blood leaks back in the wrong direction, the atrium (top chamber) increases in size and volume, the ventricle (bottom chamber) gets larger, the leak gets worse, atrial pressure increases, and congestive heart failure results (see congestive heart failure client education for a detailed description).
Elevated pulmonary artery pressure, also known as, pulmonary hypertension, develops in a subgroup of dogs with degenerative valvular disease. This is usually mild to moderate, occasionally requiring medical intervention. Dogs with severe pulmonary hypertension are typically symptomatic showing exercise intolerance, syncope (fainting), or even right heart failure (fluid accumulation around the lungs or in the abdomen). Severe pulmonary hypertension carries a grave prognosis and an associated poor quality of life.
Common clinical signs seen with advanced valvular disease include coughing, labored breathing, syncope, and/or a distended abdomen. Physical exam findings conveyed to pet owners by their veterinarian may include a heart murmur, an extra heart sound or gallop, an irregular heart rhythm (arrhythmia), abnormal pulse quality, and/or abnormal lung sounds (i.e. crackles).
Treatment ranges from no medications in the asymptomatic stages to various classes of drugs aimed to decrease pressures within the heart in advanced stages. These drugs include diuretics, vasodilators, and positive inotropes (see congestive heart failure client education for a detailed description). Prognosis is largely dependent on the underlying stage of the disease. Dogs may remain in the asymptomatic class for years. Average life span with conventional therapy (i.e. diuretic and an ace inhibitor) once in heart failure is ~1 year. Recent studies suggest with the addition of newer drugs, average life span may surpass 1.5 years.
Mitral Valve Disease
In mitral valve disease, the valve that separates the left atrium from the left ventricle is affected. The valve is present to prevent backflow of blood when the heart contracts. As the valve degenerates fluid leaks back up into the atrium, or top chamber of the heart. This causes an overload of volume and with time the pressures increase and the chambers enlarge. If fluid leaks into the lungs (pulmonary edema) congestive heart failure is present. An echocardiogram identifies the abnormal valve and backward flow. It also allows assessment of the heart function. Radiographs (X-ray) allow assessment of the lungs and it is used to determine if congestive heart failure is present. Prognosis varies from dog to dog. Some animals remain stable for years where as others will progress rapidly. We cannot cure mitral valve disease and unfortunately it is a progressive disease. Mitral valve disease is medically managed and the goal of therapy is to help the patient feel better and live longer than if no therapy was instituted.
Arrhythmias
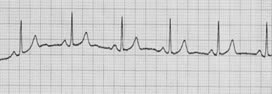
An arrhythmia is defined as an abnormal heart rhythm. The heart rhythm may be too fast (tachycardia), too slow (bradycardia) or irregular. Some arrhythmias are benign and others may be life threatening, requiring immediate care. Arrhythmias may be related to a problem with the electrical conduction system imbedded within the heart, systemic illness, electrolyte disturbances or trauma.
Arrhythmias are detected by recording an electrocardiogram (ECG, EKG). An ECG is a graphic representation of the electrical activity within the heart, detected by electrodes placed on the body. An ECG is a non-invasive diagnostic tool which does not require sedation or anesthesia. A typical ECG is recorded over 3-5 minutes. Occasionally, a patient will warrant longer monitoring of the heart rhythm. This is accomplished with telemetry (in hospital continuous monitoring of the ECG), Holter monitoring (out patient continuous monitoring of the ECG) or Event monitor (out patient monitoring which records when patient has symptoms). See ECG below.
Arrhythmias may cause weakness, collapsing, congestive heart failure or sudden death. Arrhythmias may be controlled with medications or in some instances pacemaker implantation.
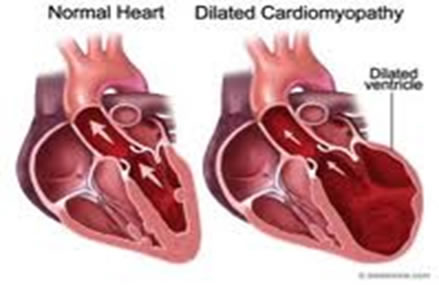
Dilated Cardiomyopathy
Dilated cardiomyopathy (DCM) is a disease of the heart muscle that causes the heart to contract poorly and become dilated over time. This disease most commonly affects large or giant breed dogs such as Doberman Pinschers, Newfoundlands, Great Danes, and Boxers. Cocker Spaniels are also predisposed to development of DCM, although any dog can develop the disease as well as some cats. This change can eventually lead to congestive heart failure, which can include fluid accumulation in the lungs (pulmonary edema), around the lungs (pleural effusion), and/or in the abdomen (ascites).
Dilated cardiomyopathy can be diagnosed by an echocardiogram (ultrasound of the heart). Pulmonary edema and pleural effusion can be diagnosed with chest x-rays. Treatment of congestive heart failure secondary to DCM includes medications such as furosemide, enalapril, and pimobendan. Pimobendan is a relatively new medication that helps the heart to contract better, which can improve quality of life, as well as life span. DCM can also be associated with cardiac arrhythmias which can exacerbate congestive heart failure and can sometimes cause sudden death. Arrhythmias often can be diagnosed by an electrocardiogram (ECG) performed in the hospital. Sometimes it is necessary for an animal to wear a 24 hour ambulatory ECG (Holter monitor) to detect arrhythmias and determine how to treat them. Some hospitalized patients have continuous telemetry to monitor their heart rhythm to help identify arrhythmias and monitor response to therapy.
Various antiarrhythmic medications can be used for treatment. Although dilated cardiomyopathy is associated with a poor long term prognosis, with the appropriate therapy and monitoring, we can help these patients have a good quality of life for as long as possible.
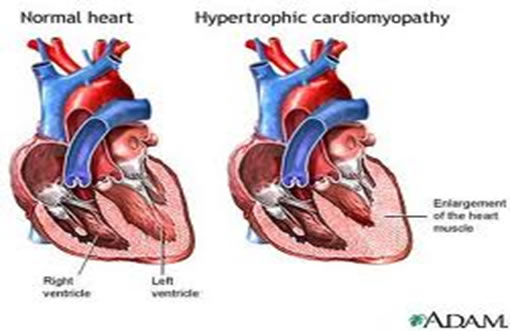
Hypertrophic Cardiomyopathy
Hypertrophic cardiomyopathy (HCM) is a rare form of heart muscle disease in dogs. It is characterized by a thickening of the walls of the heart, which leads to an inadequate amount of blood being pumped out into the body when the heart contracts during the systolic phase (pushing blood out into the arteries). When the heart relaxes between contractions during the diastolic phase (taking blood in from the vessels), an insufficient amount of blood will fill the chambers of the heart. Ultimately, HCM often will lead to congestive heart failure.
This disease, although extremely rare to dogs, usually affects young male dogs that are younger than three years old. There is also a higher incidence of the disease in mature Boston Terriers.
Most dogs with HCM will not exhibit any symptoms of the disease. If your dog is symptomatic, it will exhibit signs of congestive heart failure. These include exercise intolerance, shortness of breath, coughing, and a bluish discoloration of the skin. Very rarely, a dog with HCM may experience a transient loss of consciousness, or fainting, during a high level of activity or exercise. During a physical veterinary examination, a dog with HCM may exhibit systolic heart murmur, and a heart gallop. Unfortunately, in most cases, the most commonly reported clinical sign of HCM is sudden, fatal heart failure.
The cause of HCM in dogs is largely unknown. Although some genetic abnormalities in gene codings for certain proteins have been detected in humans and cats with the disease, no such evidence exists for dogs.
Diagnosis of HCM through medical tests is relatively difficult and involves a number of procedures. Radiographic findings may either return normal results, or may show an enlargement of the left ventricular and atrium. If a dog with HCM has left-sided congestive heart failure, there will be a buildup of fluid in the lungs. An electrocardiogram (EKG) will typically reveal normal results as well, but sometimes, it may show abnormal ST segments and T waves. Blood pressure measurements also will usually return normal results. An examination of the heart using echocardiograph (ultrasound of the heart) imaging is required for a confirmed diagnosis of HCM. In dogs with severe HCM, the echocardiograph will reveal thickened left ventricular walls, papillary muscle enlargement, and an enlarged left atrium.
Congenital Heart Disease
Congenital anomalies are diseases that the patient is born with. Patent ductus arteriosus (PDA) is the most common congenital heart defect in dogs, while ventricular septal defect is the most common congenital heart disease in cats.
Congestive Heart Failure
Congestive heart failure is the end result of severe heart disease which produces congestion and edema, poor tissue perfusion, and possibly low blood pressure.
Heart failure is referred to as left or right sided. Some animals have both left and right heart failure. Left heart failure stems from an increase in left heart pressures, which produces fluid accumulation in the lungs (pulmonary edema). Right heart failure arises from increased right heart pressures and manifests as fluid accumulation around the lungs (pleural effusion), in the abdomen (ascites) and/or in the tissues under the skin (peripheral edema). Some signs of congestive heart failure include: coughing, labored breathing, syncope (fainting), and a swollen abdomen.
Initial evaluation consists of a thorough physical examination by a veterinarian with special attention given to the cardiovascular system. At the exam, the veterinarian will inspect the animal’s gum color, pulse quality, heart sounds, heart rate and rhythm and lung sounds. Physical examination abnormalities may include pale/blue gums, weak or irregular pulses, a heart murmur, extra heart sounds, fast heart rate, irregular heart rhythms, dull lung sounds or pulmonary crackles (suggesting fluid in the lungs).
If heart disease or congestive heart failure is suspected, additional testing may be recommended, such as blood pressure measurement, chest x-rays, an electrocardiogram (ECG) and an echocardiogram (ultrasound of the heart). Testing is performed to help devise a therapeutic plan and to decipher prognosis.
Treatment of congestive heart depends on the stability of the patient. In an emergency setting, common treatment modalities may include oxygen therapy, intravenous diuretics to decrease fluid retention, vasodilators to decrease blood pressure, and positive inotropic drugs to help a weakly contracting heart pump more efficiently. Chronic treatment of heart failure involves similar drug therapy, for which the main difference is medications are administered by mouth and supplemental oxygen is usually not necessary.
The prognosis associated with congestive heart failure largely depends upon the underlying cause and stage of the heart disease.
Heartworm Disease
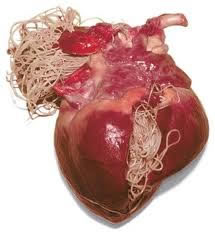
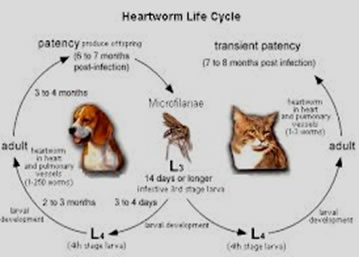
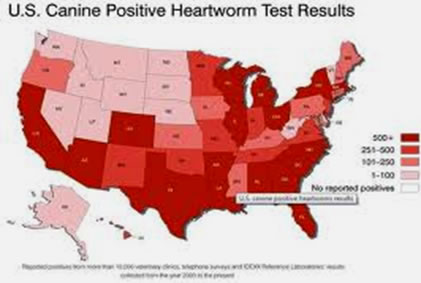
Heartworm disease is a serious and potentially fatal condition caused by parasitic worms living in the arteries of the lungs and occasionally in the right side of the heart of dogs, cats and other species of mammals, including wolves, foxes, ferrets, sea lions and (in rare instances) humans.
Heartworm disease is spread when a mosquito which has taken a blood meal from a heartworm-infested host feeds on a naive pet, injecting immature worms (called microfilaria) into the patient. The microfilaria grow, develop and travel to the pulmonary arteries as they mature. When the adult worms mature, they start producing immature worms that can serve as a reservoir of infection for other naive pets. Clinical signs associated with heartworm disease include coughing, labored breathing, exercise intolerance, collapse and sudden death.
Heartworm disease can be prevented by administering monthly heartworm preventive drugs. Unfortunately, some patients do not receive these medications and become infested with heartworms. Dogs infested with heartworms are treated with drugs to kill the microfilaria (), as well as drugs to kill the adult worms (adulticide). When the worms die off they can lodge in the lungs in large clumps (pulmonary thromboembolism) and obstruct blood flow to the lungs. This obstruction can be a life threatening event.
DIAGNOSTIC MODALITIES USE IN CARDIOLOGY
Electrocardiogram (ECG or EKG)
An electrocardiogram is used to assess the heart’s electrical activity. Electrocardiogram is non-invasive and does not require shaving or sedation. Probes are attached to the skin and waveforms are produced. The doctor is able to look at these waves and determine how the electrical conduction system of the heart is working. An electrocardiogram can be performed for many reasons, but the most common reason is if an arrhythmia is suspected.

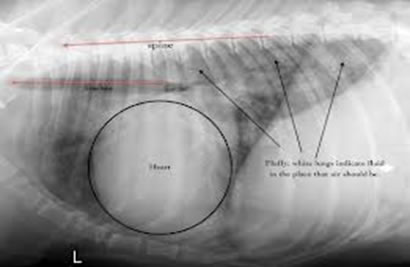
Radiographs (x-Rays)
Radiographs, or x-Rays, are made to evaluate the heart’s shape and size, as well as to assess the condition of the lungs. Making a radiograph is the only test that can diagnose pulmonary edema or congestive heart failure. It does not assess heart function.



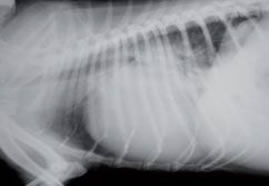
These two chest radiographs show severely enlarged hearts and
pulmonary edema (fluid) in the lungs.
Echocardiogram (echo)
An echocardiogram is an ultrasound of the heart. It allows the doctor to evaluate not only the heart size but also the heart function. It also enables visualization of the heart valves, heart muscle and chambers. Several views are obtained from both the right and left sides of the chest. Echocardiogram is non-invasive and usually does not require shaving or sedation. An echocardiogram is performed when a murmur or arrhythmia is detected during physical examination. While it is an excellent diagnostic tool, it is not the only test that may need to be performed.
Doppler Study
Doppler echocardiography allows the doctor to track the blood flow through the heart and great vessels. Doppler imaging measures the velocity of blood flow and, based on the color, it is used to determine whether the flow is normal (laminar) or turbulent. Pressures within the heart and great vessels also can be determined using the velocity measured. Doppler measurements are commonly performed during the echocardiogram.
Canine Dermatology
A small number of the most common conditions that we see are presented below. There are many other significant dermatological diseases that are not presented. If your dog has a skin condition you are concerned about please call our office for an appointment!
Flea Allergy Dermatitis (FAD)
Flea allergy dermatitis is one of the most common skin conditions in dogs. Signs are often seasonal with warm weather but can be year round here in California. Skin lesions include itchiness, raised red nodules, crusting, red inflamed skin, hair loss, and darkened skin. These lesions are most commonly found on the tail head, lumbar area, back of the thighs, and abdomen. Other skin problems like other allergies, infections, and external parasites may present with similar lesions. Often visualization of fleas and their excreta can be seen to aid in the proper diagnosis. In some allergic animals the effects of flea bites may last for weeks.
Treatment includes flea control for all animals within the household with an adulticide flea control product. In heavily infested environments fleas may continue to “emerge” for many months. In these environments a flea control product with an insect growth regulator (IGR) may be considered. Finally, the house and yard may also need to be treated to reduce the flea population. Dogs with FAD should have a monthly flea control applied on a year round basis in California. If the itching is severe, injectable or oral corticosteroids are used to prevent self trauma and if infection has already occurred antibiotics will also be needed.


TICKS
Ticks are a common problem in our area and include Deer ticks (Ixodid), Brown dog ticks (Rhipicephalus), and the American dog tick (Dermacentor). If you take your dog to parks, walk in open space, or extensively hike with your dog a topical tick medication should be applied monthly as these ticks are always present, especially in the fall through spring. These local ticks can carry a variety of infectious diseases including Lyme disease (people too!), Ehrliciosis, and other diseases. See the distribution map and slide presentation below.
RECOMMENDED FLEA & TICK CONTROL PRODUCTS
Ear Mites
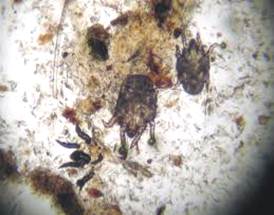
This disease is caused by an infestation by the ear mite Otodectes cynotis. This is a small mite that lives on the skin surfaces and in the ear canals.
Typically, there is a moderate to severe accumulation of dark brown/black waxy discharge from the ear canals. Often the ears are extremely itchy to the pet and frequent scratching and rubbing is noted. The scratching often results in secondary excoriations and ear canal infections with hair loss around and on the ears. Chronic head shaking and scratching can result in an ear hematoma (see below) or blood blister in the ear flap.
Ear mites are usually easily diagnosed by swab or direct visualization by our videootoscopes. Treatment includes cleaning of the debris from the ear canal with cleansers, antiparasitic medications, and often medication to treat secondary infections and the itchiness. It is important to treat all animals in the home and even any recently


ALLERGIES
Environmental (Atopy)
Canine atopy (environmental allergy) is a hypersensitivity reaction to cutaneously absorbed and possibly inhaled environmental allergens in genetically presdiposed breeds. This is a very common problem in dogs with the age of onset between 6 months and 6 years of age. In most cases the signs appear between 1-3 years.
Signs begin with skin redness and generalized itching which may be seasonal or year round depending on the causative allergen(s). The itchiness often involves the feet, flanks, axilla, face, and ears. Chronic itching and chewing usually results in hair loss, wounds with secondary infections, saliva staining in white dogs, and other chronic skin changes.
A good history is needed to try and differentiate between atopy and food allergies (below) but these conditions can occur together and are difficult to separate. Diagnostic methods include allergy testing, response to corticosteroids, while skin biopsies are non-diagnostic.
Treatments include:
- Decreasing exposure to offending allergies if possible based on allergy testing. Use of HEPA air filters hay help remove some allergens from the home environment, especially for house dust mite sensitive dogs. However, many dogs are allergic to pollens in the air that occur everywhere.
- Flea control is important to stop fleas from exacerbating the condition as many atopic dogs are also very sensitive to fleas also.
- Controlling the itching with frequent bathing, omega 3 FA’s, and corticosteroids, or other immunotherapy is an integral part of treatment.
Omega 3 FA’s may help in controlling clinical signs in up to 20% of dogs by themselves. This would be lifelong treatment and may act in synergy with other treatments. Steroids are approximately 75% effective and can eventually be tapered to lower doses to help avoid side-effects. Cyclosporine is 75%+ effective in my experience. Immuno therapy based on immune testing is 60-75% effective. It does require individualized immune vaccines to be made for each individual patient and regular injection must be given.
The prognosis for effective treatment is generally good especially if secondary conditions are controlled. Usually life-long treatments are necessary to control this condition. Treatment failures such as recurrent skin and ear infections are common due to owner compliance with treatments and failure to treat secondary conditions completely. Most client fail to understand that life-long treatment of the primary allergic condition is necessary. Dr. Innes develops a thorough and individualized plan for each individual patient including recheck appointments and telephone consultations to help manage your dogs condition and to help avoid treatment failures.
Food Allergies
Canine food allergy is an adverse reaction to a food ingredient or additive. This condition may occur at any age from puppies to elderly dogs that have been eating the same food for years. Approximately 30% of dogs with diagnosed food allergy are < 1 year of age. This condition is characterized by non-seasonal (year round) itchiness that may or may not response to corticosteroid therapy. The intense itching is often regional and includes the ears, feet, inguinal, axillary, face, and rear-end; but may be generalized. The involved skin is usually reddened and may for a coalescing rash. Chronic itching and chewing often leads to hair loss and self inflicted wounds with secondary infections of bacteria or yeast. In many dogs, recurrent skin or ear infections are the only manifestation. Of course similar lesions can result from other conditions such as atopy, ectoparasites, and primary bacterial infections, so it’s important to have a proper diagnosis!
In up to 30% of food allergy cases there may be concurrent gastrointestinal signs such as frequent bowel movements, occasional vomiting or diarrhea, and chronic flatulence.
Treatment is primarily with a hypoallergenic, elimination diet that may last 10-12 weeks. This diet must be a true prescription HA diet purchased from a veterinarian. There are some OTC diets that claim to be the same but they are not produced with the same stringent quality control measures. All treats and supplements must also be eliminated during the food trial period. One stable, if necessary, a challenge with the previous offending allergens will result in recurrence of signs within hours to days. Skin biopsies are generally not diagnostic while skin or blood testing are often not valuable either, but may help choose a proper HA diet.


Pictures of dogs with skin allergic lesions due to either atopy or food allergies.


Pictures of dogs with skin allergic lesions due to either atopy or food allergies.
Hot Spots
Hot spots or pyotraumatic dermatitis is a rapidly developing bacterial skin infection that occurs as a result of self-inflicted trauma. The lesions are a result of licks, chews, scratching, and rubbing of an area in response to an itch or pain. This problem is often seasonal and most commonly occurs during hot and humid weather. Frequently but not always, it is a result of flea bites. Hot spots are common in dogs and especially common in thick coated and long haired breeds like the Golden Retriever. The lesions are acutely itchy, rapidly enlarging areas of redness, hair loss, and weeping/oozing sores. The areas are often single, but may occur in multiple areas or coalesce to form a large lesion and are often painful to the dog. The lesions are usually found on the trunk, tail area, caudal thighs, neck, and face.
Any underlying causes such as fleas or allergies should also be identified and treated. The lesions are usually clipped and cleaned. Topical medications, systemic corticosteroids (for inflammation and itching), and antibiotics are used and lead to healing over 1-3 weeks. Elizabethan collars or other chewing deterrent are often required to assist the healing process.




These pictures are of typical “hot spot” presentations – head, trunk, and thigh areas.
Acral Lick Dermatitis
Acral lick lesions are a result of excessive, compulsive licking of a specific area on a limb. The resulting lesion is a thickened, firm, raised, ulcerated, area of hair loss. There are many reasons the licking occurs including allergies, fleas, infection, ectoparasites, arthritis, neurological pain, and trauma. Some dermatologists feel that boredom, confinement, and anxiety may be contributing factors with these lesions. These are common lesions with Doberman Pinschers, Great Danes, Golden Retrievers, Labrador Retrievers, German Shepherds, and Boxers being the most common breeds affected.
The wound usually starts as a small area of inflammation that slowly enlarges with persistent licking and chewing trauma. This resultant self-trauma results in hair loss, thickening, and an ulcerated wound. Over time a deep infection and scarring often sets in which complicates treatment and complete resolution. Treatment includes long term (6-20 weeks) of antibiotics with usual treatment 1 month beyond complete resolution of the wound, and should be based on bacterial culture and antibiotic sensitivity testing. At The Village Veterinary Hospital we are concurrently using out K-Laser to treat these lesion with other treatments leading to a much higher success rate. Occasionally, behavior modifying medications, chewing deterrents, e-collars, and muzzles may be required to stop the chewing behavior. The prognosis is variable and the more chronic lesions with deeper, extensive scarring are difficult to resolve. In many cases life-long treatment may be necessary. Early diagnosis and proper treatment are paramount to a good success rate. If your dog has lesions like those pictured below all us for an appointment so Dr. Innes can develop a proper treatment plan for your dog!


Aural Hematoma
Aural hematomas result from traumatic rupture of blood vessels in the ear flap or pinna. Chronic head shaking, rubbing, or shearing actions eventually lead to the vessel trauma, rupture, and hematoma formation. Once ruptured, the vessels bleed resulting in a blood “blister” between the skin and the supporting cartilage of the pinna. These lesions often start small and then can enlarge to involve the entire pinna by continued head shaking and subsequent further hemorrhage. If left untreated hematoma’s will slowly solidify and slowly contract into a scarred and irregular “cauliflower’ ear. These lesions are often secondary to trauma from chronic ear infections resulting from untreated allergies or improperly diagnosed and treated ear infections. Proper therapy involves treating the underlying infection. allergies, etc., and decreasing pain to stop shaking, and drainage of the lesion. If drained the lesions usually refill with fluid over time. If this occurs, the hematoma must be treated surgically. There are many different types of surgery to treat these lesions and the choice is based on experience and the size of the lesion. Once treated the lesions may also reoccur depending on the type of surgical repair employed. Dr. Innes had treated many of these cases over the years and has great cosmetic success and no recurrent lesions in the same area. This success is dependent on proper diagnosis of a primary problem such as allergies and treating both issues effectively. If your dog develops an aural hematoma call us immediately to have it cared for properly.
Classic presentation of aural hematomas.

Post-surgical appearance of aural hematoma.












